Anxiety and depression: the truth about antidepressants
If your next step is seeking professional help, their first step is almost always to put you on antidepressants.
Why? Because it’s the cheapest and easiest way for health services to deal with the situation, which doesn’t necessarily mean the best way for you.
Hard words. Yes, I know. But it’s the truth, and I believe everyone suffering from depression deserves the truth about their healing journey.
That said, read carefully what I’m writing now: I’m not discouraging you from taking antidepressants, especially if your doctor says this is your best option. It might be your best option here and now.
However, you need to know what you’re going into. You need knowledge to make the best decisions for yourself, communicate with healthcare professionals from an even ground, and get through the rougher parts of a treatment with antidepressants.

So, that’s what I’m here for. To give you the truth, as far as my personal, hard-earned experience goes.
How effective are antidepressants?
When I was in my forties, I tried several different types of antidepressants. None of them did me any favours at all. And that shouldn’t be a surprise.
A miracle medicine for everyone?
It’s hard to find straightforward information about how effective antidepressants are. The research publications aren’t always comparable. For instance, some consider the medicine effective if the patients feel slightly better, while others require the patients to feel significantly better.
However, the research papers I’ve looked at seem to place the effectiveness around 50%. That is, half of the patients feel better when they take antidepressants. Interestingly, it also seems like 30% feel better when they take placebos (‘mock medicines’).
Naturally, different antidepressants vary in how effective they are compared to placebo. According to the Guardian article above, the tested antidepressants are from 1.5 to 2 times more effective than ‘mock medicine’.
This seems far from a magic wand that fixes everything for everyone.
Does it matter?
Let’s presume we’re close to the truth if we say that antidepressants actually work for half of the depressed people who take them. Is this good or bad?
Well, what do they say about the difference between optimists and pessimists? For an optimist, the glass is half full. For a pessimist, it’s half-empty. I’m generally an optimist, and I’d say that a 50% chance of getting better isn’t too bad if you’re suffering from depression. If this was the whole story.

However, there is more to it. The fact that a placebo is almost as effective as most antidepressants is one thing. And we haven’t yet talked about the dark side of antidepressants: the side effects.
I’ll return to this, but let’s look at the big question first:
Can antidepressants solve our problems?
Of course not! Never! Remember to differentiate between underlying problems and symptoms.
Emotional painkillers
Depression, although most likely distressing enough, is more a symptom that something is wrong than the underlying problem itself.
Imagine if you broke your arm. Powerful painkillers, such as codeine, can help you cope with the pain. However, the underlying problem is a fractured bone, and codeine won’t fix that. What you need to heal is a plaster cast and time.
If an antidepressant makes you feel better (that is, you are among the lucky 50%), it is nothing more than an emotional painkiller. It will never fix the underlying problems, for instance, living in a toxic relationship or having a crap job.
Why do we get depressed?
Several articles could be written about this by people with much more psychological knowledge than me. But this is how I see it:
Emotional disorders, such as depression and anxiety, very rarely just appear in us for no reason. For most of us, they emerge because something has happened to us, just like most physical injuries. For instance, we can break an arm because you fall off the bike. And we can suffer from anxiety after a traumatic childhood.
If we look at depressions in particular, I believe most of them appear when we feel defenceless towards what happens to us. When we feel helpless, our brains put us in a ‘freeze’ state, a ‘battery saving’ low mood and low energy mode, until the circumstances improve.
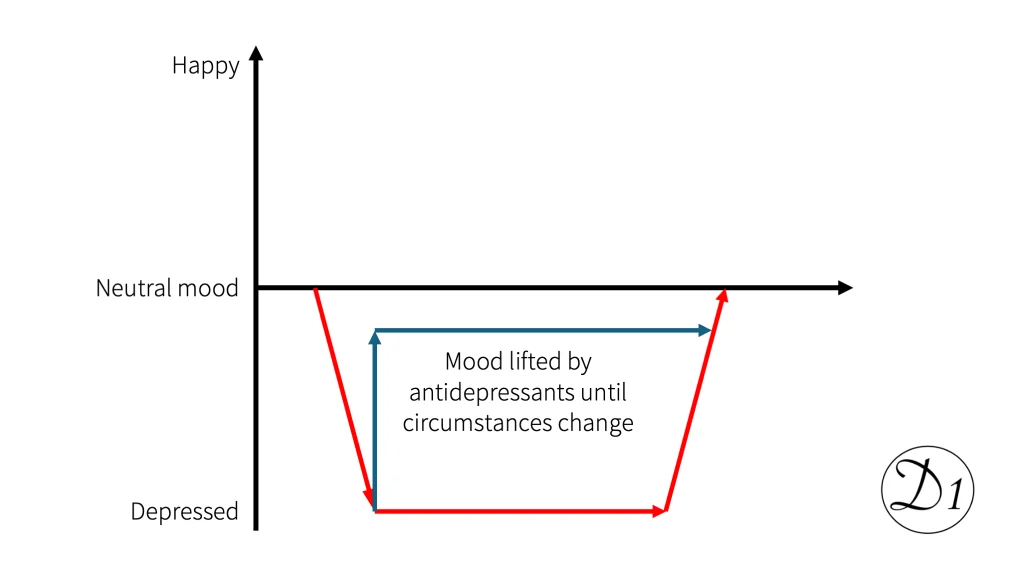
So, at their best, antidepressants can lift our mood a little bit until the circumstances improve—that is, until the underlying problems are solved. And sometimes, that’s enough.
Depressive episodes
Yes, sometimes, we’re just temporarily knocked off our feet. For instance, if a relationship breaks up or if a dear friend dies, we need time to grieve. In the meantime, our brains might try to protect us by doing its ‘freeze’ routine; a depression creeps upon us.
However, most depressions are depressive episodes. Something happens to us, and the depression starts. We process what’s happened (on our own or with help), and the depression ends. A depressive episode may last a few months, on average, about half a year.
If there is a relatively straightforward connection between something happening to us and our depression, and if we know about an antidepressant that works for us, then it makes perfect sense to use it to lift our mood a little while we are waiting for our natural healing to do its job. This is exactly like taking painkillers while our arm heals inside the plaster cast.
But some depressions aren’t one-off, time-limited episodes.
Chronic depression
If depression lasts and lasts, or if a depressive ‘episode’ is just one episode of a never-ending series, there is most likely trauma in our pasts that we haven’t resolved.
This isn’t like a fractured bone that just needs time to heal on its own. Unresolved trauma is something that must be actively faced and processed. Antidepressants can’t fix this for us. In the worst case, we might use antidepressants to numb ourselves to avoid facing our trauma and, thereby, prevent our healing.
So, no, antidepressants will never solve any problems. If we’re lucky, they can make problem-solving a little easier. But they will never be anything more than an emotional painkiller.
Are antidepressants ‘happy pills’?
When antidepressants started to be widely known in the 1980s, they were quickly given the label ‘lykkepiller’ (‘happy pills’) in my country of birth, Norway. I believe the same happened in English-speaking countries.
This is blatantly misleading. Antidepressants don’t have a pleasant effect on us like recreational drugs, such as alcohol and cannabis, have. Antidepressants won’t make us ‘feel good’.
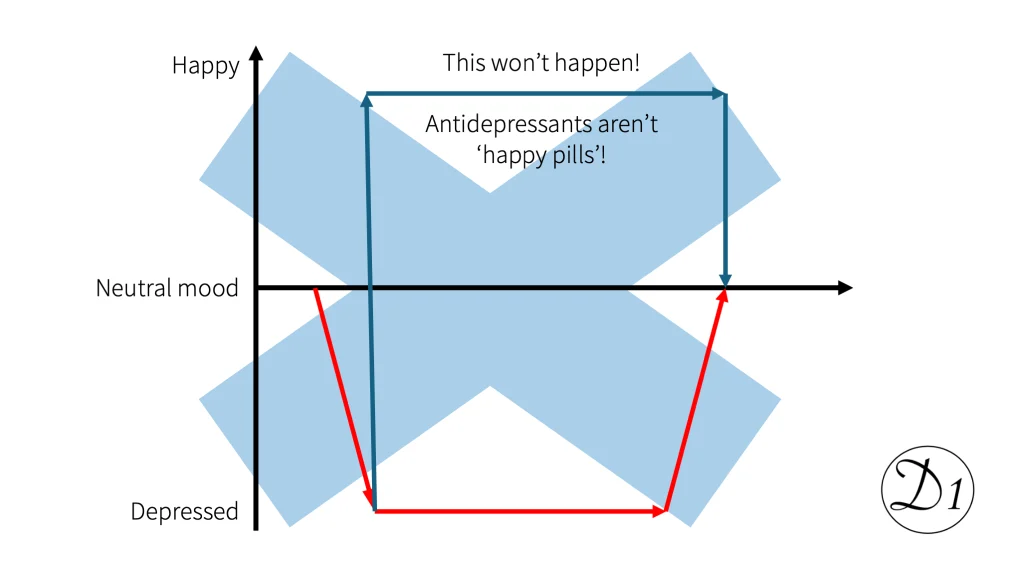
The best we can hope for is that antidepressants make us feel a little less miserable. This is done by numbing our feelings, just like painkillers numb our pain. Some people say they don’t feel anything at all while they are on antidepressants.
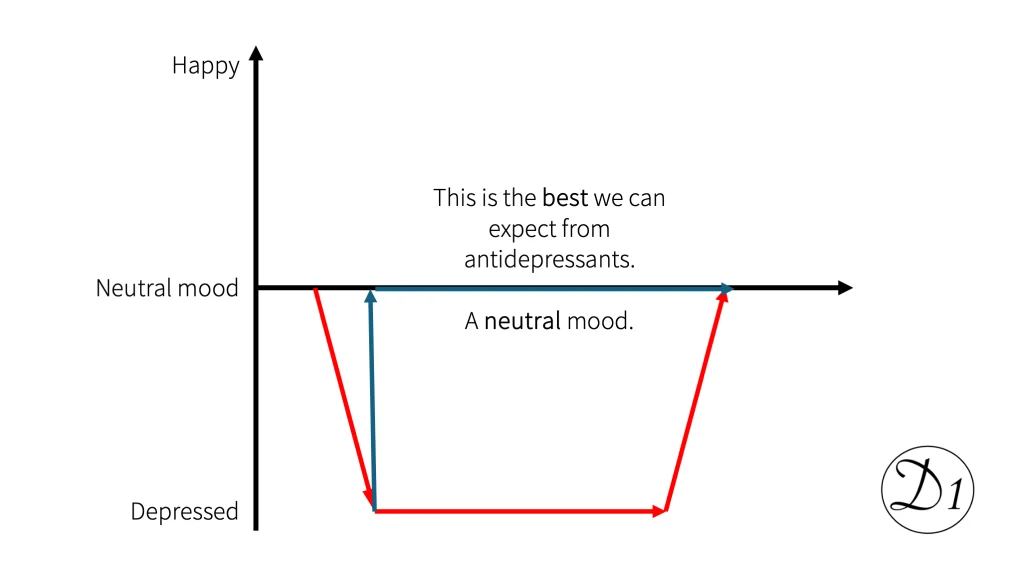
Is this good or bad? I think that depends on who we are and our situation. For some of us, feeling nothing for a period seems better than the suffering we came from. On the other hand, I have heard people say that the “emotional zombie state” the antidepressants put them in felt worse than the depression itself.
So far, we have looked at what an antidepressant realistically can do if it works for us. However, if it has an effect on us, it usually also comes with side effects.
A story about side effects
My introduction to antidepressants took place in 2005 when my Norwegian GP prescribed Cipralex for me. Something similar will happen to most people who seek professional help for depression.
SSRIs – still the antidepressants of choice
As I said at the start of the article, if we seek professional help for our depression, the first suggestion will still, in most cases, be antidepressants. Why? Because this is the quickest, easiest, and cheapest solution. For whom? Most of all, for the health services.
And the primary candidate for medication will, in most cases, be one of the SSRIs (Selective Serotonin Reuptake Inhibitors). Why? Because this is the family of antidepressants considered to work best for most people with the least side effects. Be aware that:
- Working “best” doesn’t necessarily mean working well.
- “Most people” doesn’t mean everyone.
- “Least side effects” doesn’t mean none.
Cipralex is one of many brand names for SSRIs. It’s still out there.
A selection of SSRI side effects
Back in 2005, I read the patient information leaflet I found inside my first Cipralex packet. It was about half a mile long, and much was about potential side effects. Funny thing, my GP hadn’t said a lot about this. Here is an excerpt from the side effect section of the leaflet:
- Highly common (can be experienced by more than 1 in 10 people)
- Nausea
- Headache
- Common (can be experienced by up to 1 in 10 people)
- Reduced or increased appetite
- Anxiety, restlessness, abnormal dreams, insomnia, drowsiness, dizziness, tremors.
- Diarrhoea, constipation, dry mouth
- Excessive sweating
- Changes in sexual functions
- Fatigue
- Weight gain
This is a small selection of the most common SSRI side effects. Why did I choose these? Because I had them all. Some of them faded a bit with time. Others didn’t. Weight gain is something to look out for because you don’t feel it; it just ’sneaks up on you’.

And I never had any effect from Cipralex except the side effects.
What if SSRIs don’t work?
Well, the next suggestion from the GP will most likely be an antidepressant from a different family. The suggestion for me was Effexor (sold in Norway under the name Efexor). The family name is SNRIs – you can look that up if you want to.
For me, the side effects of Effexor were horrible. The worst thing was something that felt like electric discharges in my head. I’ve seen this described as “Brain Zaps”, but it felt more like thunderbolts struck my brain.
Effexor didn’t have any positive impact on my depression either.
My last stop in the antidepressant world was Doxepin (sold under the brand name Sinequan in Norway). This is an old medicine, introduced all the way back in 1969 and belonging to the family called tricyclic antidepressants. These are known to be the worst ones when it comes to side effects.
“Mary, Mary, quite contrary.” I’m probably quite contrary in many ways; I had relatively few side effects from Doxepine. That’s probably why I stayed on it for many years. Did it help with my depression? Seen in retrospect, probably not. I had some lighter periods, but I believe now there were other reasons for that.
Important: my story isn’t necessarily your story
What you read above is my story about antidepressants and side effects. You might try an SSRI and find relief from your depression without any noticeable side effects. However, I believe you are among the lucky few if this is your story.
What we do know by now is this:
- One particular antidepressant doesn’t work for everyone. It’s about a 50% chance that it will be effective for you. However, there are other antidepressants you can try.
- Antidepressants almost always come with some side effects. How many and how hard they are varies from person to person. Side effects sometimes fade with time, sometimes not.
What does this mean? It means that getting relief from antidepressants can be:
A long and winding road
It can take a lot of time!

A slow ascent
Depending on which antidepressant you start on, your GP might put you on a small dose first and then increase slowly to the expected necessary dose for you. This slow ascent is done to try to minimise the initial side effects.
For most antidepressants, several weeks of treatment on an appropriate dose are necessary before you can expect to feel any better. If you don’t feel any improvement after, say, a month, the GP might conclude that the ‘standard dose’ isn’t enough for you and start a new, slow ascent up to the maximum dose. Spoiler alert: Higher doses usually mean more side effects.
I ended up on the maximum dose every time. My liver is a hyperactive organ, and laughed at the standard doses. I reached the maximum dose after weeks and months of slow increase. Without much success, to be honest.
Anyway, weeks and months will pass, and perhaps you won’t achieve any relief on the maximum dose either. Time to try a different antidepressant?
A slow descent
Well, it’s not that easy. First, you will have to do a slow descent to get the old one out of your system without too many withdrawal symptoms. My most memorable descent was when I weaned off Effexor. My brain was ‘zapped’ every other minute.
Finally, you can start repeating the whole cycle with a slow ascent on the new antidepressant. How many months have gone past by now?
Yes, I know, I did a third repetition of the procedure with a third antidepressant as well. Took me some years, all in all.
Would I do it again?
Rewind to 2005, in a parallel universe
Let’s say, in this parallel universe, that the first conversation with my GP had been like this:
GP: “I would recommend Cipralex. It makes things easier for about half of the patients who try it.”
Me (being an optimist, seeing a half-full glass): “Those odds aren’t too bad. I’ll try it.”GP: ”It will take at least a month, sometimes longer, before you can expect to feel any better.”
Me (being a realist): “Well, I’ve waited for 40 years already. It still doesn’t sound that bad.”GP: “Most people will experience side effects. Some experience more of them, and others less. Let me go through them with you.”
Me (after a while): “Bloody hell, that’s quite a list. But I think it’s worth a try anyway.”
Yes, I would have made the same choice if time had suddenly been rewound to 2005. Because I rarely give up before everything that can be tried has been tried. And if the first conversation with my GP had been like this, I would have been much better prepared for what happened afterwards. But I might not have tried the second and third antidepressants.
And let’s imagine we stay in the parallel universe and rewind time further back. To be precise, let’s go back to two minutes before the conversation above:
GP: “Depressions always come from somewhere, you know. Has something significant happened in your life lately?”
Me: “Not that I know of. And, to be honest, I’ve felt like this for decades.”GP: “In that case, there is a possibility we’re dealing with some bigger, underlying problems. You will need to figure out what they are. I can help you find the best way to handle this, but it will take some time. In the meantime, I will recommend an antidepressant for you. This may make things easier for you until you find and address the real problem, but it won’t solve the problem itself. Do you understand?”
Me: “Yes. Sounds okay to me.”
Back to reality
If you are very, very lucky, you meet a GP who will take the time to talk like this. For most of us, this is far from the reality.
Remember, if it seems your GP’s just trying to fob you off, it doesn’t necessarily mean they don’t care. Well, some of them don’t. We can’t expect GPs to be different from others, and a certain percentage of people just don’t have any empathy or ability to see things from your perspective.
However, it’s also possible that the clinic is underfunded and understaffed, like many clinics are, and the GP feels they need to get you out of the office as quickly as possible to make room for the next patient.
You should also consider the possibility that the GP knows a lot about depression but has learned everything from books and has no personal experience. The GP might be an empathetic person, but a lack of real-life experience makes understanding your situation harder.
Finally, you should know that much of the information available to GPs about antidepressants comes from the pharmaceutical industry itself. Antidepressants are sold for about $19 billion worldwide every year (this is more than £14 billion).
Antidepressants are a huge goldmine for pharmaceutical corporations. They have absolutely no interest in telling the nuanced, whole truth about antidepressants.
So what can you do?
You must look after yourself and not accept everything people say at face value.
I know, I know, that’s not easy if you’re suffering from a suffocating depression. However, I hope I’ve made the truth about antidepressants more visible to you. Armed with the truth, you can try to prepare yourself for discussing questions like these when you seek professional help:
- What can the underlying problems that triggered your depression be?
- Where can you find help if it’s challenging to identify and untangle the underlying problems?
- What can you realistically hope to achieve if you decide to try antidepressants? Is it to make the situation manageable until you can address the underlying problems?
- Ask for help to watch out for and handle probable side effects, such as weight gain.
- What is the exit strategy? When is it time to say ‘enough’? When and how can you decide that antidepressants aren’t going to help you or the costs of the side effects are more significant than the benefits you gain from them?
Stay strong. You are stronger than you feel when you’re under the iron heel of a depression. I wish you all the best.
Most of the pictures of people used in this article are AI-generated illustrations. Some of them resemble me, but aren’t real pictures. The exception is the picture of me from 2008.















Post Comment
You must be logged in to post a comment.